Coxarthrosis affects the hip joints of middle-aged and elderly people. The causes of its development are previous injuries, congenital and acquired diseases of an inflammatory or non-inflammatory nature. The leading symptoms of coxarthrosis are pain in the hip joint, morning swelling and stiffness of movement. At the initial stage of the pathology, treatment is conservative. If it is ineffective against the background of rapid progression of coxarthrosis or its late detection, surgical intervention, usually endoprosthetics, is indicated.
Description of the pathology
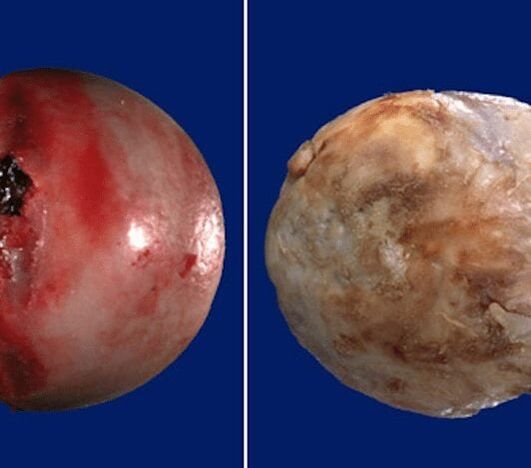
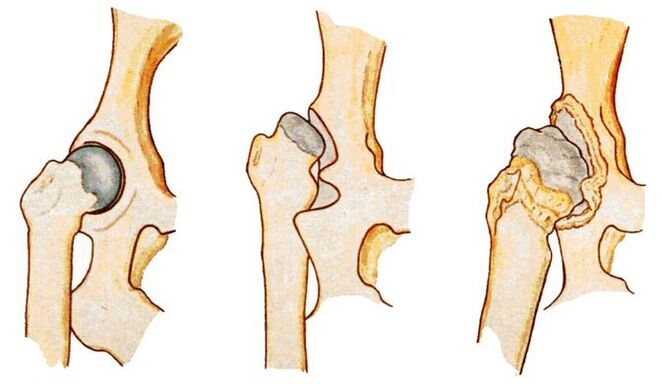
Coxarthrosis (osteoarthrosis, arthrosis deformans) is a degenerative-dystrophic pathology of the hip joint. At the initial stage of development, the structure of the synovial fluid changes. It becomes viscous, thick, and therefore loses its ability to nourish hyaline cartilage. Due to dehydration, its surface dries out and becomes covered with multiple radial cracks. In this condition, hyaline cartilage does not soften shocks well when the bones that form the joint come into contact.
To adapt to the increased pressure that occurs on them, bone structures are deformed with the formation of growths (osteophytes). Metabolism in the hip joint deteriorates, which negatively affects the muscles and ligamentous-tendon apparatus of the joint.
Degrees
Each stage is characterized by its own symptoms, the severity of which depends on the degree of narrowing of the joint space and the number of bone growths formed.
| Severity of coxarthrosis | Characteristic symptoms and radiographic signs |
|---|---|
| First | The joint space is narrowed unevenly, and single osteophytes have formed around the acetabulum. Mild discomfort occurs, but more often the disease is not clinically manifested |
| Second | The joint space is narrowed by almost 2 times, the head of the femur is displaced, deformed, enlarged, and bone growths are found even outside the cartilaginous lip. Hip pain becomes constant and is accompanied by significant limitation of mobility |
| Third | Complete or partial fusion of the joint space, multiple bone growths, expansion of the femoral head. The pain occurs day and night and spreads to the thighs and legs. Movement is possible only with the help of a cane or crutches |

Causes of the disease
Primary coxarthrosis is a destructive-degenerative lesion of the hip joint, the causes of which have not been established. This means that no prerequisites for premature destruction of hyaline cartilage were identified. The following pathological conditions can provoke secondary coxarthrosis:
- previous injuries - fracture of the femoral neck or pelvic bones, dislocation;
- hip dysplasia;
- aseptic necrosis of the femoral head;
- congenital hip dislocation;
- inflammatory, including infectious diseases of the joint (rheumatoid, reactive arthritis, gout, tendinitis, bursitis, synovitis).
Prerequisites for the development of coxarthrosis are obesity, increased physical activity, a sedentary lifestyle, metabolic disorders, hormonal disorders, kyphosis, scoliosis, and flat feet.
Symptoms of the disease
At the initial stage of development, coxarthrosis can manifest itself only with mild pain. They usually occur after intense physical exertion or a hard day at work. The person attributes the deterioration in health to muscle "fatigue" and does not seek medical help. This explains the frequent diagnosis of coxarthrosis at stages 2 or 3, when conservative therapy is ineffective.
Limitation of joint mobility
The range of motion in the hip joint is reduced due to compensatory growth of bone tissue, damage to the synovial membrane, and replacement of areas of the articular capsule with fibrous tissues devoid of any functional activity. Mobility may be somewhat limited even with grade 1 coxarthrosis. Difficulties arise when performing rotational movements with the leg.
As the disease progresses, morning stiffness and joint swelling become common. To regain mobility, a person has to warm up for several minutes. By lunchtime, the range of movements is restored, including as a result of the production of hormone-like substances in the body.
Crunch
When walking, flexing and (or) extending the hip joint, clicks, crunching, and crackling sounds are clearly heard. The reason for this sound accompaniment of each step is the friction of bone surfaces, including osteophytes, against each other. Crunching can also appear in normal health due to the collapse of carbon dioxide bubbles in the joint cavity. Coxarthrosis is indicated by its combination with dull or sharp pain.
Pain
Painful sensations become constant already at stage 2 of coxarthrosis. Their severity decreases somewhat after a long rest. The pain intensifies during the next relapse or the development of synovitis (inflammation of the synovial membrane) that often accompanies osteoarthritis. During the remission stage, the discomfort decreases somewhat. But as soon as a person becomes hypothermic or lifts a heavy object, severe pain appears again.
Muscle spasm
Increased tension in the skeletal muscles of the thigh occurs with coxarthrosis for several reasons. First, the ligaments weaken. The muscles spasm to hold the head of the femur in the acetabulum. Secondly, increased tone often accompanies inflammation of the synovial membrane. Thirdly, when osteophytes are displaced, nerve endings are compressed, and muscle spasm becomes a compensatory reaction to acute pain.
Lameness
In the later stages of development of coxarthrosis, the patient begins to limp severely. Changes in gait are provoked by flexion contractures and deformation of bone surfaces, making it impossible to maintain a straight leg position. The person also limps to reduce the severity of pain by transferring body weight to the unaffected limb.
Leg shortening
Shortening of the leg by 1 cm or more is typical for coxarthrosis of grade 3. The reasons for the decrease in the length of the lower limb are severe muscle atrophy, thinning and flattening of cartilage, narrowing of the joint space, and deformation of the femoral head.
Diagnostic methods
The initial diagnosis is made based on the patient’s complaints, external examination, medical history, and the results of a number of functional tests. Many inflammatory and non-inflammatory pathologies are disguised as symptoms of coxarthrosis, so instrumental and biochemical studies are carried out.
X-ray examination
The stage of coxarthrosis is determined by performing an X-ray examination. The resulting images clearly show destructive changes in the hip joint. This is a narrowing of the joint space, deformation of bone surfaces, and the formation of osteophytes.

CT scan
CT scan is prescribed to patients to determine the degree of flattening and deformation of hyaline cartilage. The results of the study also make it possible to assess the condition of the ligamentous-tendon apparatus, nerve trunks, muscles, small and large blood vessels.
Magnetic resonance imaging
MRI is one of the most informative studies in the diagnosis of coxarthrosis. To identify circulatory disorders in the area of the affected joint, it is performed with contrast. A routine study is prescribed to determine the degree of damage to the ligaments and deformation of the femoral head, and to detect areas of fibrous degeneration of the articular capsule.

Leg length measurement
Before the measurement, the doctor asks the patient to stand up and straighten his legs as much as possible. To obtain the most reliable data, the orthopedist uses two bone landmarks. Upper - the anterior axis of the pelvic bone, located on the anterior lateral surface of the abdomen at the outer edge of the inguinal ligament. The second reference point is any bone structure of the knee, ankle, or heel. Measuring leg length may not be informative if coxarthrosis affects two hip joints at once.
Laboratory research
Clinical blood and urine tests are performed to assess the patient's general health. And the results of biochemical studies often make it possible to detect pathologies that caused the development of coxarthrosis. Gouty arthritis is indicated by high levels of uric acid and its salts. An increase in the erythrocyte sedimentation rate and an increase in the number of leukocytes indicate the occurrence of an inflammatory process (bursitis, arthritis, synovitis). To exclude rheumatoid arthritis, rheumatoid factor, C-reactive protein, and antinuclear antibodies are determined.

Hip puncture
Using a puncture, synovial fluid is collected to study its composition and detect changes in consistency. If an infectious-inflammatory process is suspected, further biochemical examination of a biological sample is indicated.
Treatment options
When determining treatment tactics, the orthopedist takes into account the severity of coxarthrosis, the form of its course, the causes of development, and the severity of symptoms. Patients are often recommended to wear bandages with rigid ribs and orthoses from the first days of treatment. The use of orthotic devices helps slow cartilage breakdown and bone deformation.
Medicines
In the treatment of deforming arthrosis, drugs of various clinical and pharmacological groups are used. These are nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, glucocorticosteroids, chondroprotectors, ointments and gels with a warming effect.
Blockade
To relieve acute pain that cannot be eliminated by NSAIDs, intra-articular or periarticular drug blockades are prescribed. To carry them out, hormonal agents are used. The analgesic effect of glucocorticosteroids is enhanced by their combination with anesthetics.
Injections
Intramuscular injection of NSAID solutions allows you to eliminate severe pain in the hip joint. To relax skeletal muscles, a drug is usually used, which, in addition to a muscle relaxant, includes an anesthetic. In the form of injections, therapeutic regimens include B vitamins, drugs to improve blood circulation, and chondroprotectors.
Diet therapy
Overweight patients are advised to lose weight to slow the spread of pathology to healthy joint structures. The calorie content of the daily menu should be limited to 2000 kilocalories by excluding foods high in fat and simple carbohydrates. Nutritionists recommend that all patients with coxarthrosis adhere to proper nutrition. The diet should contain fresh vegetables, fruits, berries, cereal porridges, fatty sea fish, and dairy products. Following a therapeutic diet stimulates strengthening the immune system and improving overall health.
Exercise therapy and massage
In the treatment of coxarthrosis, classic, acupressure, and vacuum massage are used. After several sessions, blood circulation in the hip joint improves and nutrient reserves are replenished. Carrying out massage procedures stimulates the strengthening of the ligamentous-tendon apparatus and the restoration of soft tissues damaged by displacement of osteophytes.
Regular exercise therapy is one of the most effective ways to treat osteoarthritis. A set of exercises is compiled by a physical therapy doctor individually for the patient, taking into account his physical fitness.
Physiotherapy
Patients with coxarthrosis are prescribed up to 10 sessions of magnetic therapy, laser therapy, UHF therapy, UV irradiation, and shock wave therapy. The therapeutic effect of the procedures is due to improved blood circulation, acceleration of metabolism and regeneration processes. To relieve acute pain, electrophoresis or ultraphonophoresis with glucocorticosteroids, anesthetics, and B vitamins is performed. Applications with ozokerite or paraffin help eliminate discomfort.

Surgical intervention
If conservative treatment is ineffective, pain that cannot be eliminated with medication, or the steady progression of coxarthrosis, patients are advised to undergo surgical intervention. The operation is performed immediately in case of pathology of 3rd degree of severity, since it is impossible to eliminate the resulting destructive changes in cartilage and bones by taking medications or exercise therapy.
Arthroplasty
The operation is performed using general anesthesia. The head of the femur is removed from the acetabulum. Visible destructive changes in tissue are corrected - bone growths are removed, articular surfaces are leveled, tissue that has undergone necrosis is excised. During surgery, cavities are formed and filled with ceramic implants.
Endoprosthetics
Hip replacement with an implant is performed under general anesthesia. To prevent the development of an infectious process, a course of antibiotics is prescribed. After 10 days, the sutures are removed and the patient is discharged from the medical facility. At the rehabilitation stage, patients are shown physiotherapeutic and massage procedures, exercise therapy.
Possible consequences
At the final stage of the pathology, flexion and adduction contractures develop. The patient's leg is constantly bent, so he uses a cane or crutches to move. After complete fusion of the joint space, immobility occurs, the patient cannot do housework, and becomes disabled. Coxarthrosis is often complicated by aseptic necrosis of the femoral head, arthrosis of the knee joints, and arthritis.
Prevention and prognosis
Only grade 1 coxarthrosis responds well to conservative treatment. In other cases, endoprosthetics allows you to completely restore the functional activity of the hip joint. After installation of the endoprosthesis, the patient quickly returns to an active lifestyle.
To prevent the disease, orthopedists recommend giving up smoking, abusing alcoholic beverages, doing physical therapy and gymnastics daily, and losing excess weight if necessary.



































